Spring Always Returns
I remember the woman standing behind me, gently sobbing as I gave my deposition. I can’t recall a single detail of her face, but the sound of her anguish is as fresh as if it happened yesterday.
The attorneys’ questions brought me back to the night, almost a year earlier, that my ambulance crewmates and I rolled on the “head injury” call. Two teen boys were in a back alley, both drunk and had been fighting. The cop on scene directed us to the kid with the lacerated forehead, shooed his friend away, and went back on patrol.
As we hoisted the injured young man into our rig, his friend reappeared and tried to climb in. I struggled to keep him out until finally the officer returned and took him away in handcuffs.
En route to the hospital, our young patient told us that earlier in the day he’d tried to kill himself. He rolled up his sleeves and showed us the deep cuts on both arms. We logged it and informed the E.R. staff upon arrival. But somehow, tragically, they failed to keep him under suicide watch and released him a few hours later.
The next day he, his friend and their respective girlfriends got together and killed themselves. The incident made national headlines and led to a spate of copycat attempts that thankfully were, for the most part, unsuccessful.
Traumatic Aftermath
In the immediate aftermath, I struggled with what I would later learn in therapy was survivor’s guilt—recriminating myself that somehow, unrealistically, I could have done something different that night to have prevented the senseless tragedy. It also didn’t help when another ambulance corps member (not one of my crew) flippantly remarked: “You should be happy! Now there’s four less troublemakers to deal with.” Those insensitive words cut like a knife and only deepened my remorse.
After a few days, that remorse gradually diminished. That is, until the deposition.
The mother of one of the kids had filed a lawsuit against the hospital as well as the municipality, and even though my crewmates and I had acted appropriately, we still had to individually give sworn testimony. The interrogatories, combined with her sobs, flashed me back to that night in the alley, to feelings of guilt and despair in believing that I'd somehow failed to protect those four young lives.
My symptoms began that night and continued every night thereafter: waves of depression and anxiety, accompanied by extreme nausea that I could not alleviate by reading, watching tv or listening to popular music. My sleep was horrible, which made me perpetually irritable. It felt as though I’d been enveloped by a cold, grey, Winter shroud from which there was no hope of a Spring thaw. I sought medical help and was scoped, stuck, poked and probed but doctors found nothing wrong.
A Tough Diagnosis
That’s when I was told the problem was likely a form of post-traumatic stress.
It was tough to hear. “I’m a First Responder,” I told myself, “I’m supposed to be able to handle stuff like this! What’s wrong with me?”
After several more nauseating, sleepless nights, I finally acquiesced and hooked up with an excellent therapist. I also turned to my faith, eschewing the pop music for a Christian radio station at night, and speaking with a local church pastor. Those psychological and spiritual interventions helped me to develop a healthier perspective: that there was nothing I could have done to prevent what happened, and that I was never truly alone, even in the depths of my emotional turmoil.
The nausea and sleeplessness soon began to subside as I came to accept that my crewmates and I really did the best we could.
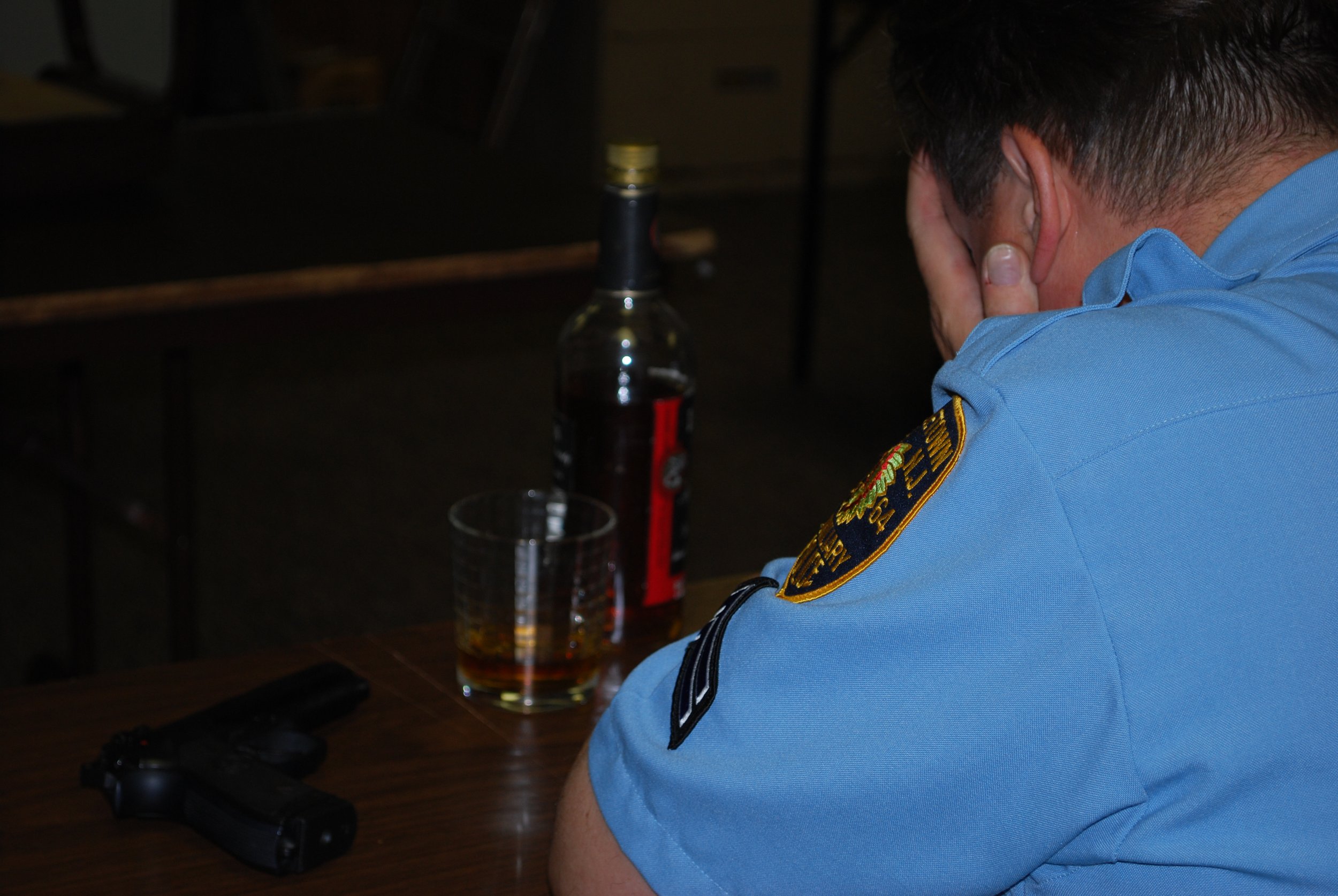
PTSD among First Responders
In my case, I had a relatively mild form of post-traumatic stress. There are many other First Responders—cops, firefighters, EMTs and paramedics—who experience far worse on the job...from fatal traffic accidents to shootings, catastrophic housefires and serious medical emergencies. Police officers, for example, are 71% more likely to develop Post-Traumatic Stress Disorder (PTSD) than civilians. Firefighters and EMS workers are also at significantly higher risk.
In my work with First Responders, Veterans and active military members, and frontline healthcare workers, there is a common thread that runs through most of them. Part of it is the mission to serve others, be it country or community. The other is a sense of honor: to never give up, to never fail their comrades, patients or constituents.
But with those virtues comes a conundrum: sometimes, despite our best efforts, rescues fail. Innocent people get hurt or die. And good people suffer. Given the right conditions, almost any First Responder can become enveloped in the bleak shroud of post-traumatic stress.
Escaping the Shroud
The good news is that in most cases, that shroud isn’t permanent. Often, time is the ultimate healer, because the further removed you become from a traumatic incident, the less affected you are by it. In other cases, extra help may be needed.
Psychological traumas are essentially existential: experiences that are so horrific they challenge our perceptions of the world, about ourselves and our place in it. Traumas can trigger in us narratives that the we and our loved ones aren’t safe, that there is no security.
There are several proven treatments for PTSD and other forms of post-traumatic stress. One that I offer my clients is Eye Movement Desensitization and Reprocessing (EMDR), which as its name implies, helps a client to become less emotionally distressed by a traumatic memory through systematic exposure to it, thereby reducing and even eliminating symptoms. Other techniques, including Cognitive Behavioral and Dialectic Behavioral therapies, are also effective.
Are you a First Responder struggling to cope with a tough call? Do you feel caught in the shroud? My hope and prayer are that you’ll reach out for help if you need it. And that you find encouragement in knowing that, in the words of Abraham Lincoln, “this, too, shall pass.”
Spring always returns.